Your Doctor's Cholesterol Test Is Worthless: The Cardiovascular Time Bomb Hiding in "Normal" Numbers
Why standard LDL testing is a 30-year-old relic that's quietly killing men over 45
Your doctor just called with your lab results. "Great news! Your cholesterol is perfect. Total cholesterol 190, LDL 110. Keep doing what you're doing. See you next year."
You hang up feeling relieved. One less thing to worry about. Your heart is healthy. No heart attack risk here.
Here's what I need you to understand: Your doctor just told you absolutely nothing useful. And the test they ran is dangerously, catastrophically outdated.
Despite those "perfect" numbers, you could have thousands of inflammatory particles tearing through your arteries right now. You could be five years away from a heart attack. And that basic cholesterol test your doctor relies on? It will never, ever catch it.
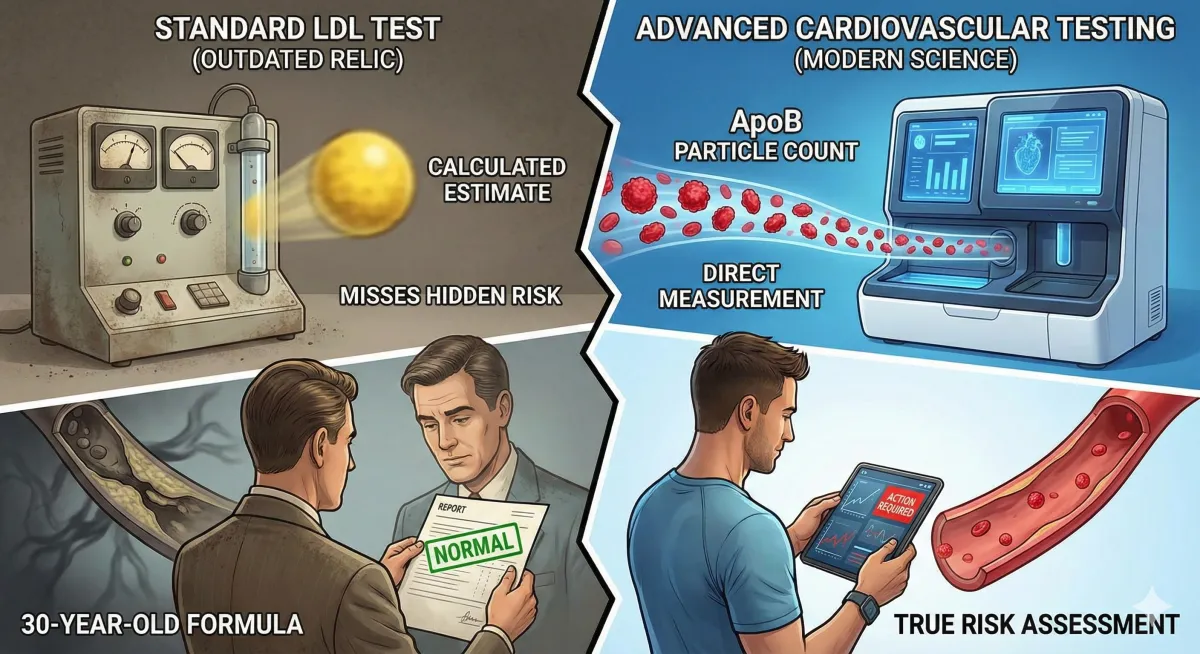
I'm going to show you exactly why the standard lipid panel is medical theater—a relic from the 1980s that gives both you and your doctor a completely false sense of security. More importantly, I'm going to show you what's actually causing heart disease, what you should be measuring instead, and why your "normal" LDL cholesterol means absolutely nothing about your actual cardiovascular risk.
This isn't some fringe theory. This is established science that's been published in major cardiology journals for over a decade. The American Heart Association knows it. Top cardiologists know it. But somehow, your primary care doctor is still ordering the same worthless test they learned about in medical school thirty years ago.
Let's fix that.
The Wake-Up Call: When "Perfect" Cholesterol Nearly Kills You
Mark was 48 years old. Successful executive. Trained four times a week—never missed a workout. Ate what everyone calls "clean." Chicken breast, vegetables, olive oil. No family history of heart disease. Did everything right.
His annual physical showed total cholesterol of 185, LDL cholesterol of 98, HDL of 62, triglycerides of 88. His doctor actually used the word "perfect." Told him whatever he was doing, keep it up. Gave him a literal pat on the back.
But Mark came to see me because despite these "perfect" numbers, something felt off. He was gaining belly fat despite training hard. His energy was declining. He wanted optimization, not just a clean bill of health from someone checking boxes.
We ran advanced lipid testing—the kind most doctors either don't know about or don't bother ordering. Here's what we found hiding beneath those "perfect" basic numbers:
LDL particle number: 2,847. Should be under 1,000. He had nearly triple the number of LDL particles he should have.
Small LDL particles: 92%. Should be under 30%. Almost all of his particles were small, dense, and dangerous—the kind that penetrate artery walls and cause plaque buildup.
ApoB: 148 mg/dL. Should be under 100. This is the actual protein that causes atherosclerosis, and his was 50% higher than optimal.
Lp(a): 87 nmol/L. A genetic risk factor that increases heart attack risk by 2-3x. He had no idea he carried this.
Let me translate what this means in plain language: Mark was at massive cardiovascular risk. Not borderline. Not "something to watch." Massive. Despite what his "perfect" basic cholesterol test said, he was on a direct path to a heart attack in his 50s. Maybe sooner.
We implemented a personalized protocol based on his genetics. Turns out he has ApoE4, which explained why his particle number was sky-high despite reasonable LDL cholesterol. Three months later, his LDL particle number dropped to 1,124—still not perfect, but out of the danger zone. His small particles dropped to 31%. His ApoB normalized to 96.
We probably prevented a heart attack.
Here's the kicker: His basic LDL cholesterol barely changed. It went from 98 to 94. If we'd only measured standard cholesterol like most doctors do, we would have missed everything. He would have walked away thinking he was fine. And in five years, he might have dropped dead on a morning run.
This isn't a rare case. This is happening to men every single day. Men with "normal" cholesterol who trust their annual physical, who think they're doing everything right, who have no idea they're walking around with a cardiovascular time bomb.
Your basic cholesterol test is not protecting you. It's giving you false reassurance while the real damage accumulates silently.
The Fundamental Lie: Why Standard Cholesterol Testing Measures the Wrong Thing
Let me explain what your doctor is actually measuring when they run a "lipid panel." They're measuring total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. Four numbers. That's it. And based on these four numbers—which tell you almost nothing about actual risk—they determine whether you're at risk for heart disease or not.
Here's the problem: They're measuring the amount of cholesterol. But what actually causes heart disease is the number of particles carrying that cholesterol.
This is not a subtle distinction. This is everything.
Think about it like this: LDL particles are cars on a highway. Cholesterol is the passengers inside those cars. Standard LDL testing counts the passengers. Advanced testing counts the cars. Why does this matter? Because the cars are what cause traffic jams in your arteries, not the passengers. The cars—the actual LDL particles—are what penetrate your artery walls, get oxidized, trigger inflammation, and build the plaques that eventually rupture and cause heart attacks.
You could have few cars with many passengers—low particle number but high cholesterol. You're fine. Or you could have many cars with few passengers—high particle number but "normal" cholesterol. You're in serious danger. Standard testing cannot tell the difference.
Let me give you a real-world example. Two men, both 47 years old, both come in with LDL cholesterol of 130 mg/dL. Slightly elevated by standard guidelines. Their doctors both say the same thing: "Your LDL is a bit high. Let's watch it. Try to eat less saturated fat."
Man A has 800 LDL particles. That's optimal—under 1,000. His particles are large and fluffy. They don't easily penetrate artery walls. He's at low cardiovascular risk despite the slightly elevated LDL cholesterol number.
Man B has 2,500 LDL particles. That's more than double what it should be. His particles are small and dense. They slip right through artery walls, get oxidized, and trigger the whole inflammatory cascade that builds plaques. He's at very high cardiovascular risk despite having the exact same LDL cholesterol as Man A.
Same LDL cholesterol. Same doctor advice. Opposite cardiovascular risk.
Man B needs aggressive intervention immediately. Man A is fine. But standard testing can't tell them apart. They both walk away with the same useless advice about eating less saturated fat. And in ten years, Man B has a heart attack while Man A is playing tennis.
This is not theoretical. This is published, peer-reviewed science. The Framingham Offspring Study followed thousands of people for decades and found that LDL particle number predicted cardiovascular events far better than LDL cholesterol. The Multi-Ethnic Study of Atherosclerosis studied nearly 7,000 participants and confirmed the same thing. When particle number and cholesterol amount disagreed, particle number was right about risk.
The research is clear. The science is established. And yet your doctor is still ordering the wrong test.
What Actually Causes a Heart Attack: The Real Mechanism Your Doctor Isn't Explaining
Let me walk you through what's actually happening in your arteries right now. Not the simplified story about "bad cholesterol" clogging your pipes. The real mechanism.
Step one: LDL particles circulate in your bloodstream. Some of them—particularly the small, dense ones—slip between the cells lining your artery walls. This is called endothelial penetration. Large particles are too big to fit through easily. They bounce off. But small particles? They slide right through. The more particles you have, the more chances for penetration. More particles equals more risk. Period.
Step two: Once those LDL particles are inside your artery wall, they get trapped. They can't get back out. And while they're stuck there, they get damaged by free radicals—a process called oxidation. Oxidized LDL is inflammatory. Your body recognizes it as foreign, dangerous, something that needs to be attacked.
Step three: Your immune system sends in white blood cells called macrophages to clean up the mess. These macrophages engulf the oxidized LDL particles. They gorge themselves on oxidized cholesterol until they become bloated "foam cells." These foam cells accumulate, more immune cells show up, smooth muscle cells migrate to the area, and a fibrous cap forms over the whole mess. Congratulations, you now have an atherosclerotic plaque.
Step four: Over years or decades, that plaque grows. It can stay stable for a long time. But eventually—triggered by inflammation, stress, a blood pressure spike, who knows—that plaque ruptures. The fibrous cap tears. The contents of the plaque spill into your bloodstream. Your body sees this as a massive injury and forms a blood clot to patch it. That blood clot blocks blood flow to your heart. Heart attack.
Here's the critical insight your doctor isn't telling you: The number of LDL particles determines how many particles enter your artery wall in the first place. More particles means more opportunities for penetration. More penetration means more oxidized LDL. More oxidized LDL means more inflammation and plaque buildup. More plaque means higher risk of rupture and heart attack.
The amount of cholesterol inside those particles? Almost irrelevant to the process. What matters is particle count and particle size. That's it. That's what drives atherosclerosis. And that's exactly what standard cholesterol testing doesn't measure.
Your doctor is measuring cholesterol amount—the passengers. But they should be counting particles—the cars. They're using a test that was developed in the 1970s, standardized in the 1980s, and hasn't fundamentally changed since then. It's a 50-year-old test that measures the wrong thing. And they're using it to make life-or-death decisions about your cardiovascular health.
This is medical malpractice by obsolescence.
The Three Numbers That Actually Matter (And Your Doctor Isn't Checking)
If LDL cholesterol is worthless, what should you be measuring? Let me give you the three markers that actually predict cardiovascular risk. These aren't experimental. These aren't fringe. These are published in major cardiology journals, recommended by the American Heart Association, and used by every lipidologist and preventive cardiologist who knows what they're doing.
Marker One: LDL Particle Number, or LDL-P. This is the actual count of LDL particles in your blood. It's measured by NMR spectroscopy or ion mobility, technologies that separate and count particles directly. Optimal is under 1,000 nmol/L. Acceptable is 1,000 to 1,300. Anything over 1,600 is high risk. Over 2,000 is very high risk. This is the single best predictor of cardiovascular events. Better than LDL cholesterol, better than total cholesterol, better than any standard lipid marker. This should be the primary target for therapy, not LDL cholesterol. But most doctors never measure it.
Marker Two: LDL Particle Size. Not all particles are equally dangerous. Large, fluffy particles don't easily penetrate artery walls. They're relatively benign. Small, dense particles slip right through and cause damage. You want predominantly large particles. Specifically, you want less than 20% of your particles to be small. If you have "Pattern B" lipids—predominantly small particles—you're at significantly higher risk even if your LDL cholesterol is "normal." Small particles are typically caused by insulin resistance, high triglycerides, and high carbohydrate intake. The good news is particle size is modifiable through diet and lifestyle. The bad news is most doctors never measure it, so you have no idea whether your particles are large or small.
Marker Three: Apolipoprotein B, or ApoB. Every atherogenic particle—every LDL, VLDL, IDL, and Lp(a) particle—has exactly one ApoB protein sitting on its surface. This is the protein that lodges in your artery wall and starts the whole atherosclerotic process. If you count ApoB, you're essentially counting particles. Optimal is under 80 mg/dL. Acceptable is 80 to 100. Borderline high is 100 to 130. Over 130 is high risk. The American Heart Association's 2024 guidelines explicitly acknowledge that ApoB is superior to LDL cholesterol for risk prediction. Some major cardiology societies now recommend ApoB as the primary target instead of LDL-C. It's simpler to measure than LDL-P, more widely available, and highly predictive. Yet most primary care doctors still don't order it.
Let me show you how this plays out in real life. I had a client come in with LDL cholesterol of 110—perfectly normal by standard guidelines. His doctor told him he was fine. But his LDL particle number was 2,200. More than double what it should be. His ApoB was 135, well into the high-risk range. He had normal cholesterol but massive cardiovascular risk. Standard testing missed it completely. If we hadn't run advanced testing, he would have walked away thinking he was healthy. And he would have been quietly building plaques in his arteries for the next decade until something ruptured.
This is not rare. This is common. Studies show that about 20% of people with "normal" LDL cholesterol have high LDL particle numbers. One in five. And almost none of them know it because their doctors never test for it.
You could be one of them right now. Your cholesterol could look perfect on paper while you have thousands of dangerous particles circulating in your bloodstream. And you would have no idea until you're in the emergency room with crushing chest pain.
Standard cholesterol testing is medical theater. It makes you and your doctor feel like you're monitoring cardiovascular risk, but you're not. You're measuring the wrong thing and making decisions based on incomplete, misleading data.
The Hidden Genetic Risk Factor Nobody's Testing For
There's one more marker I need to tell you about. It's called Lipoprotein(a), or Lp(a). It's an LDL particle with an extra protein attached called Apo(a). This protein makes the particle both highly atherogenic—meaning it causes plaques—and highly thrombogenic—meaning it promotes blood clots. It's determined almost entirely by genetics, affects about 20% of the population, and cannot be lowered by diet, exercise, or statins.
If your Lp(a) is elevated—above 50 mg/dL or 125 nmol/L depending on the units—your risk of heart attack increases by two to four times. This is a massive risk factor. And it's completely invisible on standard cholesterol testing. Most doctors never check it. Many don't even know about it. You could carry this genetic risk your entire life and never know until you have a cardiac event.
I had a client with Lp(a) of 156 nmol/L. Very high. Genetic. He can't lower this number. It's built into his DNA. But knowing it changes everything about how we manage his cardiovascular risk. We target his LDL particle number much more aggressively—under 700 instead of under 1,000. We're more aggressive with anti-inflammatory strategies. We monitor more frequently. We take every other risk factor more seriously because we know he has this genetic strike against him.
This is critical information. And standard cholesterol testing never measures it.
About one in five people have elevated Lp(a). Most of them don't know. They go through life thinking their cardiovascular risk is average when it's actually two to three times higher. They eat reasonably well, exercise moderately, and assume they're fine. Then they have a heart attack at 52 and everyone says "it came out of nowhere." It didn't come out of nowhere. The information was there. Nobody looked for it.
You need to know your Lp(a) level. It's a simple blood test. You only need to do it once because it doesn't change. If it's elevated, you and your doctor can make informed decisions about how aggressively to manage your other risk factors. If it's normal, great—you can relax a bit. But you need to know. Not knowing is not protecting you.
Why Your Doctor Isn't Ordering These Tests (And Why That's Unacceptable)
You might be wondering: If these tests are so important and the science is so clear, why isn't my doctor ordering them? Why am I still getting the same basic lipid panel from the 1980s?
Here's the uncomfortable truth: Most doctors graduated medical school 10 to 30 years ago. Advanced lipid testing wasn't part of the curriculum. They learned "check LDL cholesterol, if high prescribe a statin, if normal you're good." That's what they were taught. That's what they know. And unless they've actively sought out continuing education in lipidology—which most haven't—that outdated knowledge is what they're still using to make clinical decisions about your health.
The major clinical guidelines haven't helped. The ACC/AHA guidelines have historically focused on LDL cholesterol as the primary target. Even though newer research clearly shows particle number is superior, guidelines change very slowly. They're updated by committees, influenced by decades of prior recommendations, and conservative by design. Doctors follow guidelines because it protects them from liability. If they do what the guidelines say and something goes wrong, they're legally covered. If they deviate from guidelines—even to use better science—they're exposed.
Then there's insurance. Insurance companies don't always cover advanced lipid testing. They consider it "not medically necessary" unless you already have known cardiovascular disease or very high cholesterol. Doctors don't want to fight with insurance companies. They don't want their patients to get surprise bills. So they order what's covered by default: the standard lipid panel. Even if it's inadequate. Even if it misses critical information.
Add in time constraints. Primary care doctors have 15-minute appointments. They're checking blood pressure, reviewing medications, ordering routine labs, discussing three other chronic conditions, and trying to address whatever brought you in that day. They don't have time to deep-dive into advanced lipid interpretation. They don't have time to explain why particle number matters more than cholesterol amount. They order the standard panel, glance at the LDL number, and move on.
None of this is necessarily their fault. The system is broken. Medical education is outdated. Guidelines lag behind research. Insurance creates perverse incentives. Time constraints make thoughtful medicine nearly impossible.
But here's what I need you to understand: None of those systemic problems protect you from having a heart attack.
The fact that your doctor is overwhelmed, under-trained in lipidology, and constrained by insurance limitations doesn't change the fact that you could have high particle numbers and massive cardiovascular risk hiding behind "normal" cholesterol. It doesn't change the fact that standard testing is inadequate. It doesn't change the fact that you need better information to make informed decisions about your health.
You cannot outsource responsibility for your health to a system that is fundamentally not designed to optimize it. Your primary care doctor is trying their best within a broken system. I'm not criticizing them as individuals. But I am telling you that relying solely on their standard testing is not enough. Not if you're serious about preventing cardiovascular disease. Not if you actually want to know your risk instead of just hoping for the best.
How to Actually Assess Your Cardiovascular Risk: What to Order and How to Read It
Let me give you the exact panel you need to order. You can request this from your doctor, or if they won't order it, you can order it yourself through online lab companies like Marek Health, Ulta Lab Tests, or Life Extension. You don't need permission. You don't need a doctor's referral. You pay out of pocket—usually $150 to $250 for a comprehensive advanced lipid panel—and you get real information about your cardiovascular risk.
Order the NMR LipoProfile from LabCorp or the CardioIQ Advanced Lipid Panel from Quest. Both measure LDL particle number, particle size distribution, and give you detailed information about your lipid subfractions. Add on ApoB if it's not included. Add on Lp(a) as a one-time test since it's genetic and doesn't change. Add hs-CRP for inflammation and homocysteine for endothelial damage. If you want to go deeper, add fasting insulin to assess insulin resistance and an omega-3 index to see your anti-inflammatory status.
Now let me show you how to interpret the results. I'm going to give you three real scenarios so you can see how misleading standard panels can be and how much information advanced testing reveals.
Scenario One: Standard panel looks fine, advanced panel reveals high risk. Basic lipid panel shows total cholesterol 195, LDL cholesterol 115, HDL 55, triglycerides 125. Your doctor says "borderline, watch your diet." But advanced testing shows LDL particle number of 2,400—more than double what it should be. Small particles are 85% of the total. ApoB is 145. This person is at very high cardiovascular risk despite borderline LDL cholesterol. They have severe dyslipidemia that standard testing completely missed. This is likely driven by insulin resistance, evidenced by the triglycerides of 125 and the predominance of small particles. They need aggressive intervention: significant carbohydrate reduction, resistance training, post-meal walks, omega-3 supplementation, possibly berberine or metformin. If we only looked at the standard panel, we'd think they're borderline and just need to "eat better." In reality, they need immediate, aggressive intervention.
Scenario Two: Standard panel looks concerning, advanced panel shows low risk. Basic lipid panel shows total cholesterol 245, LDL cholesterol 160, HDL 75, triglycerides 50. Your doctor wants to put you on a statin immediately because your LDL is "high." But advanced testing shows LDL particle number of 950—optimal, under 1,000. Small particles are only 15% of the total. ApoB is 85. This person has high LDL cholesterol but low particle numbers and predominantly large, benign particles. They're actually at low cardiovascular risk despite the high LDL-C number. They don't need a statin. They need to maintain their healthy lifestyle and monitor inflammatory markers. This pattern is common in people with ApoE2 genetics or those with excellent metabolic health—high HDL, very low triglycerides, good insulin sensitivity. Standard testing would push them toward unnecessary medication. Advanced testing reveals they're fine.
Scenario Three: The genetic wild card. Standard panel shows total cholesterol 210, LDL cholesterol 135, HDL 50, triglycerides 125. Looks average. Advanced testing shows LDL particle number 1,600—elevated, and Lp(a) of 180 nmol/L—very high genetic risk. This person has moderately elevated particle numbers plus a massive genetic risk factor. The Lp(a) alone triples their risk. Combined with elevated LDL-P, this is high to very high risk. They need very aggressive particle number reduction—target LDL-P under 700, ApoB under 70. They likely need pharmaceutical intervention, not just lifestyle changes. They need more frequent monitoring. They might need a coronary calcium score to assess current plaque burden. This is someone who needs specialized care from a lipidologist, not generic advice from a primary care doctor. And standard testing would completely miss the Lp(a) and underestimate their risk.
These scenarios play out every single day in primary care offices across the country. People get basic panels, get generic advice, and walk away with no idea what their actual cardiovascular risk is. Some are falsely reassured when they're in danger. Some are pushed toward medications they don't need. Almost none get the nuanced, personalized risk assessment that advanced testing provides.
You deserve better information. You deserve to know your actual risk, not just a guess based on outdated markers.
What to Do If Your Numbers Are High: The Strategic Intervention Protocol
Let's say you get advanced testing done and your LDL particle number is 2,000 and your ApoB is 130. You're at high risk. Now what?
First, identify the root cause. High particle numbers don't appear out of nowhere. They're driven by specific metabolic and genetic factors. The most common cause by far is insulin resistance. High insulin drives small particle formation, increases triglycerides, and worsens your entire lipid profile. Check your fasting insulin, HOMA-IR, and HbA1c. If you're insulin resistant—fasting insulin over 7, HbA1c over 5.5%—this is priority number one. Fix insulin resistance and your lipids will improve dramatically. See our metabolic reset series for the complete protocol.
The second most common cause is high carbohydrate intake, especially refined carbohydrates. Excess carbs drive insulin resistance, increase triglycerides, and promote small particle formation. If you're eating 200 to 300 grams of carbs daily—bread at breakfast, rice at lunch, pasta at dinner—and you have high particle numbers, you need to cut carbs significantly. Target 50 to 100 grams daily if you're insulin resistant, 100 to 150 if you're not. Emphasize protein and healthy fats. This intervention alone can reduce small particles by 30 to 50% in three months.
Genetics matter too. If you have ApoE4 genetics—about 25% of people do—you're a hyper-responder to saturated fat. High saturated fat intake in ApoE4 carriers drives particle numbers up dramatically and causes inflammation. You need a Mediterranean approach: fatty fish instead of red meat, olive oil instead of butter, avocados and nuts instead of cheese. This can reduce LDL particle number by 20 to 40% in ApoE4 carriers. Get genetic testing through 23andMe for $99 and upload your results to interpretation sites to check your ApoE status. It's critical information.
Lifestyle interventions are non-negotiable. Resistance training three to four times per week builds muscle, improves insulin sensitivity, and reduces visceral fat—all of which improve lipid profiles. This can reduce particle numbers by 10 to 20%. Post-meal walks for 10 minutes after each meal reduce glucose and insulin spikes, which over time improves particle size and number. Sleep seven to eight hours every night because sleep deprivation worsens insulin resistance, which worsens lipids. Manage chronic stress because high cortisol worsens insulin resistance and increases inflammation, both of which worsen lipids.
Supplement strategically. Omega-3 fatty acids at 2 to 3 grams of combined EPA and DHA daily reduce triglycerides by 20 to 30%, reduce small particles, and provide anti-inflammatory benefits. Use high-quality, third-party tested brands that are IFOS certified to ensure purity. If you're insulin resistant, add berberine 500 mg three times daily with meals. Berberine works like metformin, improves insulin sensitivity, and can reduce particle numbers by 15 to 20%. Plant sterols at 2 grams daily block cholesterol absorption and can reduce particle numbers modestly. Red yeast rice contains natural statins and can reduce particle numbers by 15 to 25% if you're trying to avoid pharmaceutical statins, though you should supplement with CoQ10 if you use it.
If lifestyle and supplements don't get your particle numbers to target—under 1,000 for LDL-P, under 80 for ApoB—then consider pharmaceutical intervention. Statins remain the most studied and effective option for reducing particle numbers, typically by 30 to 50%. Ezetimibe blocks cholesterol absorption and reduces particles by 15 to 20%, and can be combined with statins for synergistic effects. PCSK9 inhibitors are powerful—they reduce particle numbers by 50 to 60%—but they're injectable and expensive, typically reserved for high-risk patients or those who can't tolerate other medications.
Work with a lipidologist or functional medicine provider who actually understands advanced lipids. Not all doctors are trained in particle-based management. Your primary care doctor might be great at general medicine but out of their depth with advanced lipid interpretation and particle-targeted therapy. Find someone who specializes in this. It's worth it.
Retest in three months. Track LDL-P, ApoB, small LDL-P, triglycerides, and hs-CRP. If you're not at goal, adjust the protocol—more aggressive dietary changes, add supplements, consider medication. If you're at goal, maintain the protocol and retest every six to twelve months to ensure you stay optimized. This is a long-term strategy, not a one-time fix.
Why Men Over 45 Can't Afford to Wait
Cardiovascular disease risk doesn't increase linearly. It accelerates dramatically after age 40 in men. Here's why: Atherosclerosis is a cumulative process. Every single day, LDL particles enter your artery walls. If you have high particle numbers, plaque builds slowly but relentlessly over decades. By the time you're 45, you may have significant plaque accumulation even if you feel completely fine, even if you have no symptoms, even if you can run five miles without stopping.
Your metabolic health is declining too. After 40, insulin sensitivity decreases, visceral fat increases, muscle mass decreases, inflammation increases, and testosterone declines. All of these worsen your lipid profile. You're fighting an uphill battle. The longer you wait to address high particle numbers, the more plaque accumulates, and the harder it becomes to reverse.
You don't get warning signs. Atherosclerosis is silent. You don't feel plaques building in your arteries. You don't feel your endothelium becoming dysfunctional. You feel fine right up until the moment a plaque ruptures and you have a heart attack. By then, it's too late for prevention. You're in damage control mode, hoping the ER can save you.
This is why testing matters. You need objective data. You need to know your particle numbers, your ApoB, your Lp(a). You need to know your actual risk, not your assumed risk based on how you feel or how you think you eat. Testing gives you information. Information allows intervention. Intervention prevents heart attacks.
If you're over 45 and you haven't had advanced lipid testing, you're flying blind. You're hoping your "normal" cholesterol means you're safe. You're trusting a 50-year-old test to tell you something it's not designed to measure. That's not a strategy. That's denial.
The Bottom Line: Standard Testing is Medical Negligence
Let me bring this all together. Standard cholesterol testing measures the amount of cholesterol in your blood. But particle number—the actual count of LDL particles—drives cardiovascular risk, not cholesterol amount. Two men with identical LDL cholesterol can have completely opposite risk profiles. One has low particle numbers and large particles—he's fine. The other has high particle numbers and small particles—he's in serious danger. Standard testing cannot tell them apart.
This is not controversial. This is not fringe medicine. This is peer-reviewed, published science that's been validated in multiple large-scale studies over decades. LDL particle number and ApoB are superior predictors of cardiovascular events compared to LDL cholesterol. The American Heart Association acknowledges this. Major cardiology societies recommend using particle-based markers. And yet most primary care doctors still only measure LDL cholesterol.
For men over 45, this is unacceptable. You could have "normal" cholesterol and massive cardiovascular risk. You could be years away from a heart attack and completely unaware. Your doctor might be telling you "everything looks great" while you have thousands of dangerous particles attacking your arteries.
You need advanced lipid testing. You need to know your LDL particle number, your particle size distribution, your ApoB, and your Lp(a). These markers give you real information about cardiovascular risk. They allow strategic intervention before you have a cardiac event. They can literally save your life.
You have two options: Trust your basic cholesterol test and hope your "normal" numbers mean you're actually safe. Or get advanced testing, know your actual risk, and intervene strategically if needed.
Which option would you choose?
Order advanced lipid testing this week. Request an NMR LipoProfile or CardioIQ panel from your doctor, or order it yourself through online lab companies. It costs $150 to $250. That's less than you'd spend on supplements in two months. It's less than a single night out. It's information that could prevent a heart attack.
Stop trusting outdated tests. Stop accepting false reassurance. Stop hoping for the best while doing the minimum. Get the data. Know your risk. Intervene intelligently.
Your life might depend on it.
- Dr. Arvindh
P.S. In my practice, every single client over 40 gets advanced lipid testing as part of their baseline assessment. We don't guess about cardiovascular risk. We measure it precisely, interpret it in the context of genetics and metabolic health, and design personalized protocols to optimize particle numbers—not just lower cholesterol. If you're serious about cardiovascular health, this is where you start. Join our community and let's get you the real information you need.
https://members.functionalcoremd.com/communities/groups/members/home